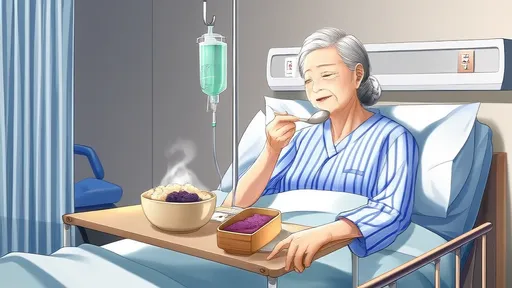
For individuals with limited mobility or those recovering from illness, eating while lying down presents unique challenges that require careful consideration. The risk of choking increases significantly when food or liquid enters the airway instead of the digestive tract. This makes proper positioning and mindful eating techniques crucial for maintaining safety during meals.
Understanding the risks associated with eating in a supine position is the first step toward prevention. When lying flat, gravity works against the natural swallowing mechanism, making it easier for food particles or liquids to stray into the trachea. The epiglottis, a small flap that normally covers the windpipe during swallowing, may not function as effectively in this position. Elderly patients and those with neurological conditions face particularly high risks due to potential swallowing dysfunction or reduced cough reflexes.
Creating the right environment for safe eating begins with proper bed positioning. Elevating the head of the bed to at least 30 degrees helps utilize gravity to direct food toward the esophagus. Specialized wedge pillows can provide additional support if adjustable beds aren't available. The dining area should be well-lit and free from distractions that might cause the person to eat too quickly or without proper attention to chewing.
Food preparation plays an equally important role in preventing aspiration. Moist foods that hold together well often prove safer than dry, crumbly textures. Cutting food into small, manageable pieces reduces the need for extensive chewing. Thickened liquids move more slowly than thin beverages, allowing better control during swallowing. Many healthcare professionals recommend consulting with a speech-language pathologist for personalized texture modification recommendations based on individual swallowing capabilities.
Caregiver techniques significantly impact mealtime safety for bedridden individuals. Maintaining eye contact helps monitor for signs of difficulty during swallowing. Encouraging small bites and complete chewing between each mouthful prevents rushing. Learning to recognize warning signs like coughing, throat clearing, or voice changes after swallowing allows for immediate intervention. Having suction equipment nearby provides an added layer of security for those at highest risk.
The psychological aspects of eating while bedridden shouldn't be overlooked. Many patients experience frustration or embarrassment about needing assistance with such a basic function. Creating a dignified, pleasant dining experience contributes to both safety and quality of life. Simple touches like using regular dishes instead of hospital trays or incorporating favorite foods within dietary restrictions can make meals more enjoyable while maintaining safety protocols.
Specialized equipment exists to facilitate safer eating in bed. Angled utensils help maintain proper wrist position when feeding oneself from a reclined position. Non-slip mats keep plates stable on bed trays. Spill-proof cups with special valves control liquid flow. For individuals with severe mobility limitations, assistive devices like long-handled or weighted utensils may provide greater independence during meals while reducing choking risks.
Hydration management presents particular challenges in bedridden patients. Dehydration thickens secretions and makes swallowing more difficult, while overhydration can lead to fluid overload in those with certain medical conditions. Frequent small sips of appropriately thickened liquids often work better than large amounts at mealtimes. Careful monitoring of intake and output helps maintain this delicate balance while preventing aspiration.
Post-meal positioning remains crucial for continued safety. Remaining upright for at least 30 minutes after eating allows gravity to assist digestion and reduces reflux risk. For patients requiring complete bed rest, a slight right-side tilt may help prevent gastric contents from flowing back toward the esophagus. Observing for any signs of respiratory distress in the hour following meals helps catch potential aspiration before serious complications develop.
Education forms the foundation of effective choking prevention programs. Both caregivers and patients need thorough training in recognizing early signs of swallowing difficulty. Regular reassessment of swallowing function ensures that dietary recommendations remain appropriate as conditions change. Many hospitals now implement formal dysphagia screening protocols for at-risk populations, significantly reducing aspiration pneumonia rates.
Emergency preparedness completes the comprehensive approach to safe eating in bed. Caregivers should receive training in basic life support and choking first aid. Having a clear emergency action plan that includes when to call for professional help prevents hesitation during critical moments. Regular drills help maintain skills that might otherwise fade between actual emergencies.
Technological advances continue to improve options for safe eating in challenging positions. From smart utensils that monitor eating pace to beds with integrated weighing systems that track nutritional intake, innovation supports traditional safety measures. However, these tools work best when combined with fundamental attention to positioning, food texture, and attentive caregiving practices developed through years of clinical experience.
The complex interplay between physical limitations, medical conditions, and nutritional needs requires individualized solutions. What works perfectly for one patient might prove ineffective or even dangerous for another. This reality underscores the importance of professional evaluation and customized care plans in achieving truly safe eating experiences for those confined to bed.

By /Aug 7, 2025

By /Aug 6, 2025
By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025